Cervical cancer is a significant global health issue, particularly in regions with limited access to vaccines and screenings. While treatments like radiation and chemotherapy help many patients, they don’t work for everyone, creating a pressing need for more effective and personalized approaches. A new study offers fresh insights into how cervical cancer develops and how it could be treated better. By combining the study of genes and proteins, known as proteogenomics, researchers are uncovering new ways to predict treatment outcomes and target the disease.
What Makes Cervical Cancer Unique?
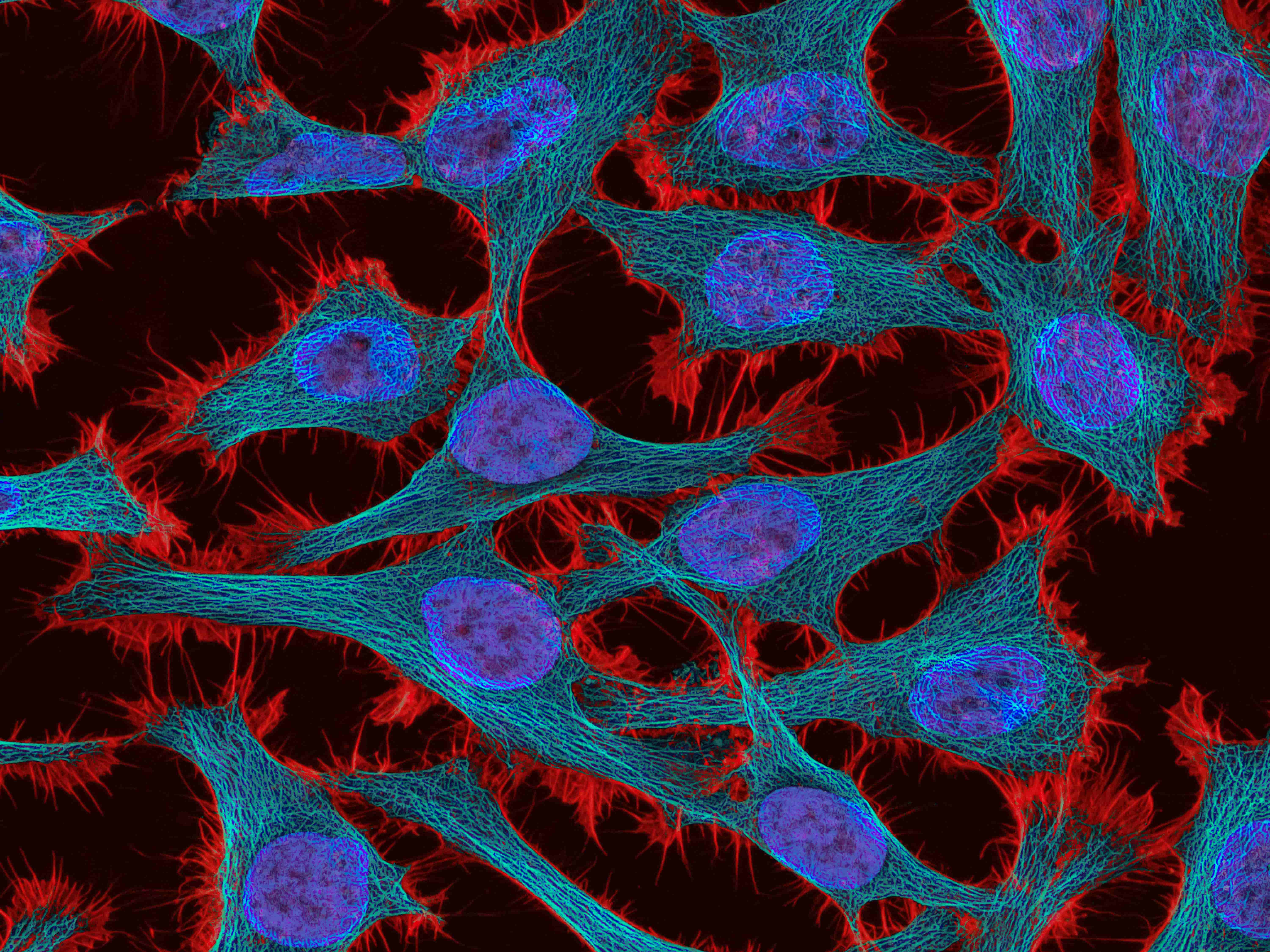
Cervical cancer is closely linked to the human papillomavirus (HPV), a virus found in nearly all cases of the disease. This study analyzed 139 tumor samples and found that HPV plays a critical role in shaping how the cancer grows and spreads. The virus alters the molecular environment of the tumor, making it harder to treat effectively. Understanding these changes is key to developing better treatments.
The research also revealed that cervical cancer is not a single disease but can be divided into three distinct subtypes. Each subtype has unique genetic and immune system characteristics, meaning that one-size-fits-all treatments might not be the best approach. Tailoring therapies to the specific type of tumor could improve outcomes significantly.
New Tools for Predicting Treatment Success
Radiation therapy is one of the most common treatments for cervical cancer, but its effectiveness varies from patient to patient. The study identified a protein called PRKCB that could help predict whether a patient will respond well to radiation. This discovery could allow doctors to make more informed decisions about which treatments to use, saving time and potentially improving survival rates.
Another key finding was the role of the EP300 protein, which helps tumors grow and spread. Targeting this protein with new drugs could provide a powerful weapon against cervical cancer, particularly in cases where other treatments have failed.
Personalized Medicine: The Future of Cancer Care
These findings highlight the potential of personalized medicine - an approach that tailors treatments to the unique characteristics of each patient’s disease. By analyzing the genetic and protein makeup of a tumor, doctors can choose therapies that are more likely to work and cause fewer side effects. This shift toward individualized care is already transforming the treatment of other cancers, and now cervical cancer could benefit too.
A Global Perspective
While cervical cancer rates are declining in wealthier countries thanks to HPV vaccination and regular screenings, the disease remains a leading cause of death in low-income regions. The insights from this study could lead to treatments that are not only more effective but also more accessible, making a difference where it’s needed most. Identifying key markers for treatment success could help healthcare providers use resources more efficiently, improving outcomes for patients worldwide.
Looking Ahead
This study is a major step forward in understanding cervical cancer, but there’s still work to be done. Future research will focus on testing these findings in clinical trials and expanding the study to include more diverse patient populations. If successful, these efforts could lead to new therapies that transform how cervical cancer is treated.
By combining advanced science with a commitment to better patient care, this research offers hope for millions of women. It’s a reminder that breakthroughs in understanding disease at a molecular level can pave the way for more effective treatments, better outcomes, and, ultimately, lives saved.