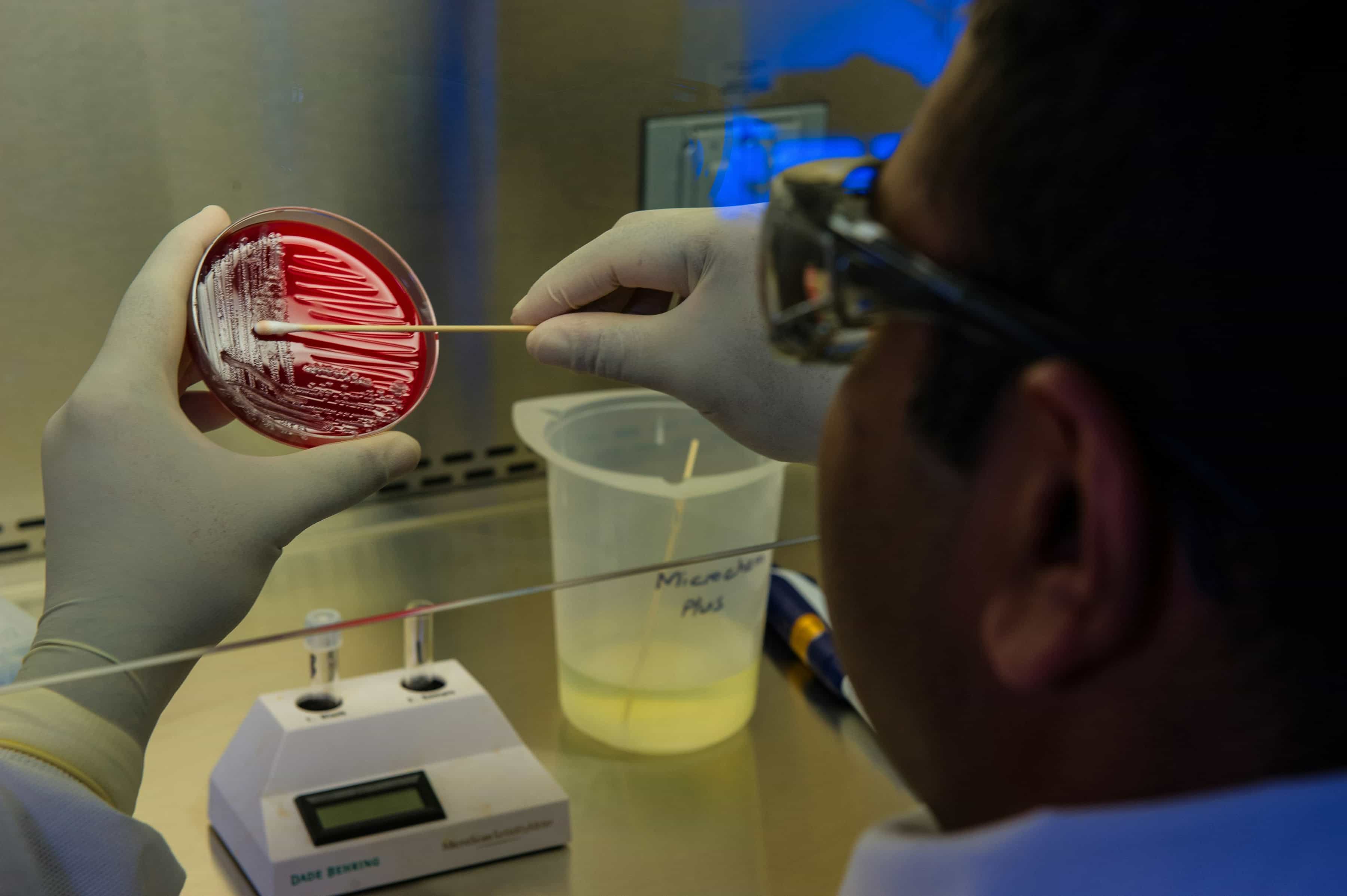
Antibiotic resistance is a growing global health crisis. As bacteria evolve to outsmart our drugs, the tools we use to fight infections must evolve too. Scientists have developed a groundbreaking approach called personalized antimicrobial susceptibility testing (AST). This method tailors antibiotic testing to each patient, offering smarter, faster solutions to treat infections like urinary tract infections (UTIs) while minimizing the rise of antibiotic-resistant superbugs.
Why Antibiotic Testing Needs an Upgrade
The current method of testing antibiotics in labs uses a “one-size-fits-all” approach. Doctors select from a standard panel of antibiotics, test them against bacteria from a patient’s sample, and use the results to decide on a treatment. However, this system has limitations. It tests drugs that might not be necessary, wastes resources, and doesn’t consider individual patient factors like prior antibiotic use or resistance patterns. The result? Treatment decisions that may not be the most effective or sustainable.
How Personalized Testing Works
This new approach uses advanced statistical models to predict which antibiotics are most likely to work for each patient. By analyzing real-world healthcare data, including the patient’s age, history of antibiotic use, and resistance patterns, the system tailors the testing process. The goal is to prioritize drugs from the World Health Organization’s “Access” category - antibiotics less likely to cause resistance.
For example, if a patient’s data suggests a high chance of resistance to certain antibiotics, those drugs are skipped in testing. Instead, the test focuses on drugs with a higher likelihood of success, saving time and resources while guiding doctors to more effective treatments.
Real-World Impact: Better Results, Smarter Choices
In simulations using data from UTI patients, the personalized method delivered more actionable results for Access antibiotics compared to the standard approach. It also ensured that patients were more likely to receive a drug that worked for their specific infection. By tailoring testing, this method provides clinicians with better information while reducing unnecessary exposure to broad-spectrum antibiotics, which can drive resistance.
The system also showed how individual factors like age, recent antibiotic use, and even the specific bacteria involved influenced drug resistance. For instance, younger patients were generally more susceptible to certain antibiotics, while prior use of a drug increased resistance risks.
The Fight Against Superbugs
Antimicrobial resistance (AMR) is one of the most pressing health threats of our time. According to the World Health Organization, over 70% of antibiotics used worldwide should ideally come from the Access category to slow the rise of resistance. The personalized AST system aligns perfectly with this goal, helping healthcare providers make better choices for both patients and the planet.
This method could revolutionize how antibiotics are prescribed, especially in low-resource settings where Access antibiotics are often more affordable and available. By focusing on precision and efficiency, the system has the potential to save lives while preserving the effectiveness of vital drugs for future generations.
A Vision for the Future
The research team envisions personalized AST becoming a standard tool in microbiology labs worldwide. With further development, this technology could expand to other types of infections and antibiotics, making it a cornerstone of modern healthcare. The approach could also integrate seamlessly into existing systems, offering a practical, cost-effective solution for hospitals and clinics.
As antibiotic resistance continues to rise, innovative tools like personalized AST offer a glimmer of hope. By combining advanced data modeling with real-world healthcare needs, this technology bridges the gap between science and practice, creating smarter, safer treatments for everyone.